
‘Embrace the Ditch,’ and Other Lessons Learned in Duke CEE’s Overture Engineering
Civil and environmental engineering students learn to design buildings within less-than-optimal parameters in a collaborative capstone course
We’re sorry, but that page was not found or has been archived. Please check the spelling of the page address or use the site search.
Still can’t find what you’re looking for? Contact our web team »
Read stories of how we’re teaching students to develop resilience, or check out all our recent news.

Civil and environmental engineering students learn to design buildings within less-than-optimal parameters in a collaborative capstone course

On a Star Wars-themed field of play, student teams deployed small robots they had constructed
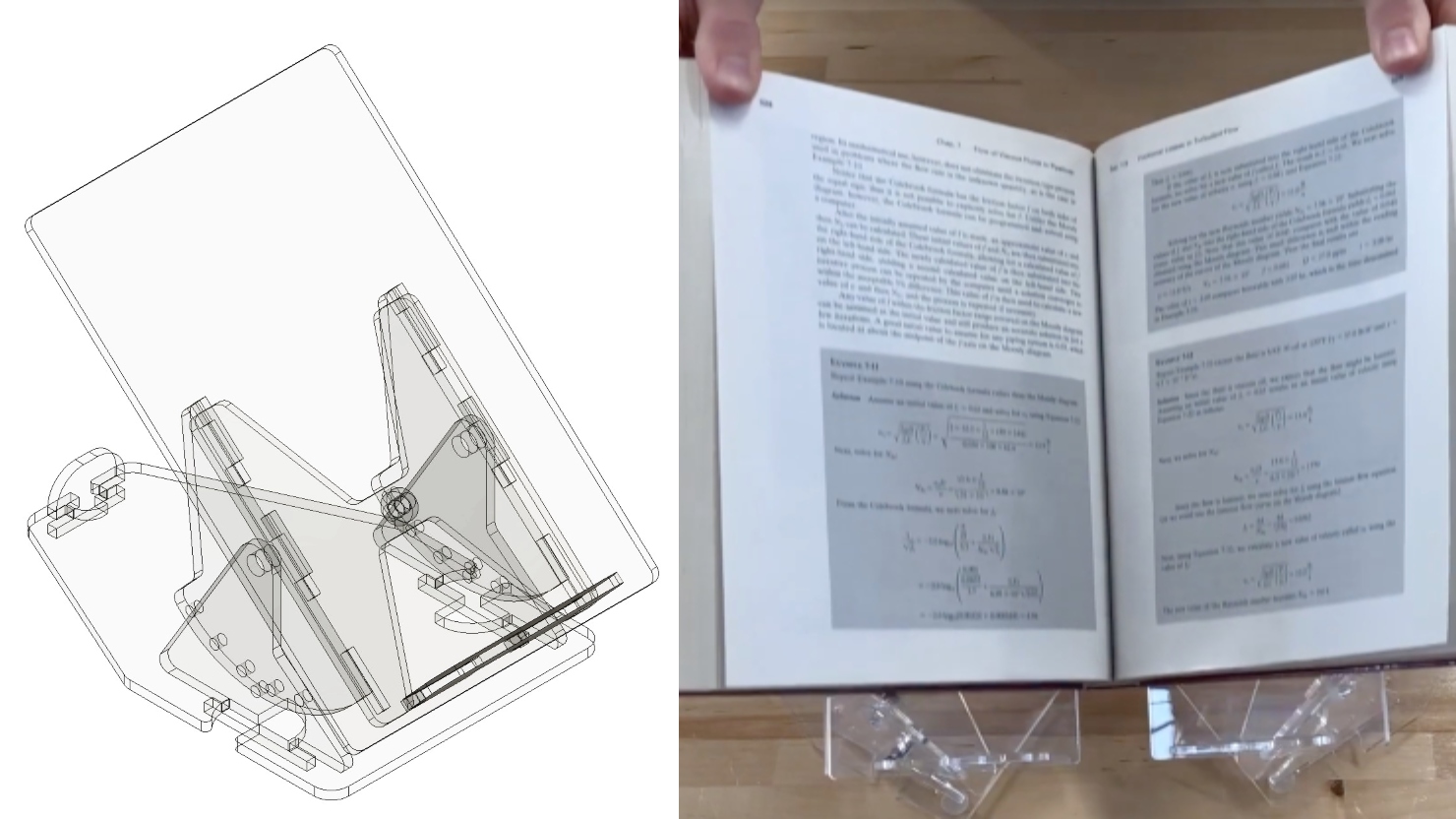
Two projects from First-Year Design course are patent-pending. Student surveys suggest the course also fosters teamwork, leadership and communication skills.
Jun 23
Jun 23
The ODE Summer Design Camp also functions as a professional development and training opportunity for middle and high school STEM teachers. Teachers are invited to participate in the camp to […]
Jun 23
The ODE Summer Design Camp is an immersive biomedical engineering design experience. Over the course of five weeks, participants will learn about the engineering design process and use it to […]